The vagus nerve plays a crucial role in our body’s overall function and well-being. As nurses, it is essential to understand the anatomy and function of this vital nerve to provide effective care to our patients. Additionally, we must be knowledgeable about the process of vagus nerve stimulation and be aware of the observations we can expect during this therapy. This article aims to provide nurses with a comprehensive understanding of what to anticipate when stimulating a patient’s vagus nerve.
Understanding the Vagus Nerve
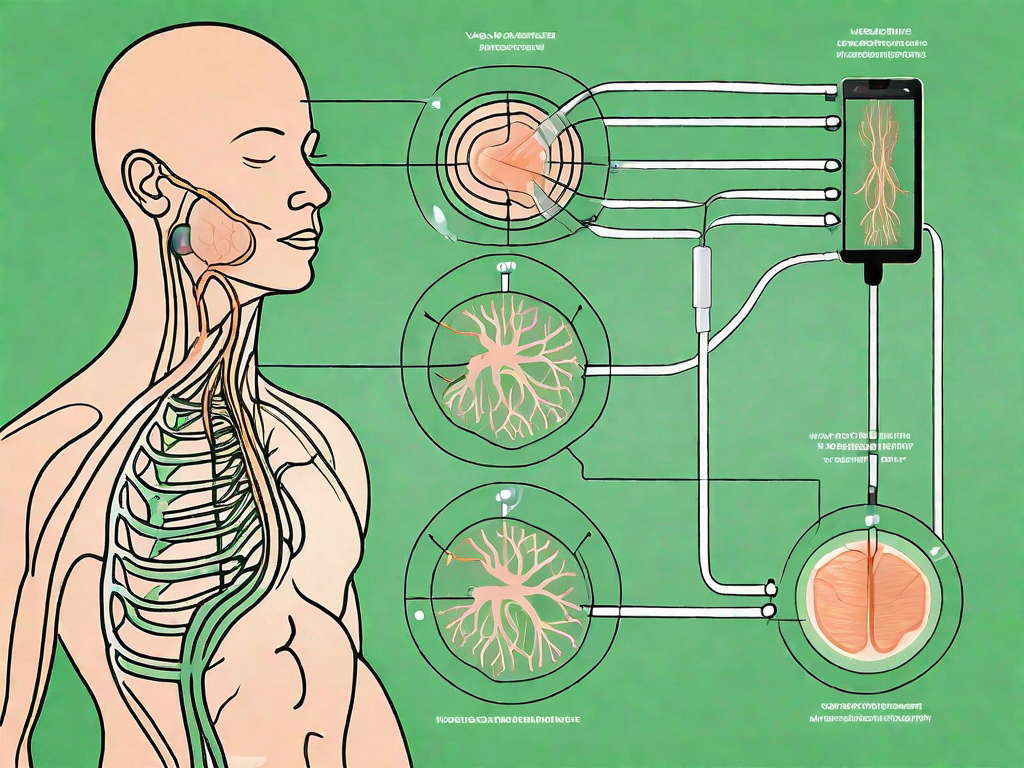
The vagus nerve, also known as the tenth cranial nerve or CNX, is one of the longest and most crucial nerves in our body. It starts in the brainstem and extends throughout various organs, including the heart, lungs, stomach, and intestines. Its primary function is to regulate the parasympathetic nervous system, which controls our rest and digest responses.
The vagus nerve, with its intricate network of fibers, plays a vital role in maintaining the delicate balance of our bodily functions. Let’s delve deeper into the fascinating anatomy and function of this remarkable nerve.
Anatomy and Function of the Vagus Nerve
The vagus nerve consists of both motor and sensory fibers, allowing it to transmit signals in both directions. Its motor fibers control the muscles involved in activities such as swallowing and speaking, ensuring the smooth functioning of these essential processes. Meanwhile, its sensory fibers relay information about our body’s internal organs back to the brain, providing crucial feedback that helps maintain homeostasis.
Imagine a complex highway system, with signals constantly flowing back and forth, ensuring that our body functions seamlessly. The vagus nerve acts as the main thoroughfare, facilitating communication between the brain and various organs.
The Role of the Vagus Nerve in the Body
The vagus nerve is responsible for regulating various bodily functions, each playing a crucial role in our overall well-being. One of its primary functions is to control heart rate, ensuring that it beats at an appropriate pace to meet the body’s demands. It also influences digestion, helping to optimize nutrient absorption and maintain a healthy gut.
But the vagus nerve’s influence extends far beyond the cardiovascular and digestive systems. It has a profound impact on our mood, influencing our emotional state and helping to regulate stress responses. When the vagus nerve is functioning optimally, it promotes a sense of calm and relaxation, allowing us to navigate life’s challenges with resilience.
Furthermore, the vagus nerve is intricately involved in our immune response. It helps regulate inflammation levels in the body, ensuring that our immune system responds appropriately to threats while avoiding excessive activation that can lead to chronic inflammation.
Interestingly, the vagus nerve also plays a role in pain perception. By modulating pain signals, it can influence how we experience and interpret pain. This intricate interplay between the vagus nerve and our perception of pain opens up exciting possibilities for therapeutic interventions.
Stimulating the vagus nerve can have profound effects on the body’s functioning and can be used therapeutically in certain medical conditions. Techniques such as vagus nerve stimulation have shown promise in treating epilepsy, depression, and even inflammatory conditions like rheumatoid arthritis.
As we continue to unravel the mysteries of the vagus nerve, its importance in maintaining our overall health and well-being becomes increasingly apparent. The more we understand this remarkable nerve, the more we can harness its potential to optimize our physical and mental health.
The Process of Vagus Nerve Stimulation
When it comes to stimulating the vagus nerve, it is important to understand the underlying science behind this technique. By gaining this knowledge, nurses can provide better care and support to patients undergoing vagus nerve stimulation therapy.
The Science Behind Vagus Nerve Stimulation
Vagus nerve stimulation involves delivering electrical impulses to the nerve, typically through a device implanted under the skin. These electrical impulses help modulate the vagus nerve’s activity, influencing the way it communicates with the brain and various organs. The exact mechanisms behind the therapeutic effects of vagus nerve stimulation are not fully understood but are thought to involve the regulation of neurotransmitters and anti-inflammatory responses.
Neurotransmitters play a crucial role in the communication between nerve cells. They are chemical messengers that transmit signals across synapses, the tiny gaps between nerve cells. By regulating neurotransmitters, vagus nerve stimulation may help restore balance in the brain and improve various physiological functions.
In addition to neurotransmitters, vagus nerve stimulation is believed to have anti-inflammatory effects. Inflammation is a natural response of the immune system to injury or infection. However, excessive or chronic inflammation can contribute to various health conditions. By modulating the vagus nerve’s activity, vagus nerve stimulation may help regulate the body’s inflammatory response, promoting healing and reducing inflammation-related symptoms.
Techniques for Stimulating the Vagus Nerve
There are different techniques for stimulating the vagus nerve, including both invasive and non-invasive methods. Invasive methods involve surgical implantation of a device, while non-invasive methods use external stimulation techniques such as transcutaneous vagus nerve stimulation. Each approach has its advantages and considerations, and nurses must be familiar with the specific method used in their patients.
Invasive vagus nerve stimulation typically involves the implantation of a small device, similar to a pacemaker, under the skin near the collarbone. This device is connected to the vagus nerve, and electrical impulses are delivered through the device to stimulate the nerve. The device can be programmed to deliver the appropriate level of stimulation for each individual patient.
Non-invasive vagus nerve stimulation, on the other hand, does not require surgery. Instead, it involves the use of external devices that deliver electrical impulses to the vagus nerve through the skin. One common non-invasive technique is transcutaneous vagus nerve stimulation, which uses electrodes placed on the skin overlying the vagus nerve. These electrodes deliver low-intensity electrical impulses, stimulating the nerve and modulating its activity.
Non-invasive methods like transcutaneous vagus nerve stimulation offer the advantage of being less invasive and more easily reversible compared to surgical implantation. However, they may require more frequent sessions and have a lower level of precision in delivering the electrical impulses.
Overall, understanding the science behind vagus nerve stimulation and the different techniques used is essential for nurses providing care to patients undergoing this therapy. By staying informed and knowledgeable, nurses can ensure the best possible outcomes for their patients and provide the necessary support throughout the vagus nerve stimulation process.
Observations During Vagus Nerve Stimulation
When patients undergo vagus nerve stimulation therapy, they may experience various physiological, emotional, and psychological responses. As nurses, it is crucial to be aware of these observations and provide appropriate support and care to our patients.
Physical Responses to Expect
During vagus nerve stimulation, patients may experience changes in heart rate, blood pressure, and respiratory rate. Some individuals may also notice improvements in digestion and a sense of relaxation. It is important to monitor these physical responses closely and adjust therapy settings accordingly.
Emotional and Psychological Reactions
Vagus nerve stimulation can also have an impact on an individual’s emotional and psychological well-being. Some patients may report improvements in mood, reduced anxiety levels, or better stress management. However, others may experience temporary side effects such as hoarseness, coughing, or tingling sensations. Being attentive to these emotional and psychological changes is essential in supporting patients throughout their therapy.
Potential Risks and Complications
While vagus nerve stimulation can be a beneficial therapy for many patients, it is important to be aware of the potential risks and complications that may arise. By identifying and managing these adverse reactions promptly, nurses can ensure the safety and well-being of their patients.
Identifying Adverse Reactions
Some patients may experience complications during vagus nerve stimulation, such as infection at the implantation site or voice changes. In rare cases, there may be a risk of seizure activity. Nurses should closely monitor patients for any signs of adverse reactions and promptly report any concerns to the healthcare team.
Managing Potential Risks
To minimize the risks associated with vagus nerve stimulation, nurses should carefully educate patients about the therapy, its potential benefits, and possible complications. Providing thorough instructions on care and maintenance of the device and ensuring regular follow-up visits are also crucial in managing potential risks effectively.
The Nurse’s Role in Vagus Nerve Stimulation
As part of the healthcare team, nurses play a critical role in the success of vagus nerve stimulation therapy. Their expertise and support are invaluable throughout the entire process, from preparing the patient for the procedure to monitoring and documenting the patient’s responses.
Preparing the Patient for Vagus Nerve Stimulation
Prior to vagus nerve stimulation, nurses must ensure that patients are well-informed about the procedure, its potential benefits, and any possible complications. They should address any concerns and provide patients with the necessary resources to make informed decisions. Additionally, nurses may need to assist in preoperative preparations and provide emotional support to help alleviate anxiety.
Monitoring and Documenting Patient’s Responses
During vagus nerve stimulation therapy, nurses must carefully monitor patients for any changes in vital signs, mood, or overall well-being. Regular assessment and documentation of the observations are essential in evaluating the therapy’s effectiveness and detecting any complications. Nurses should also ensure open communication with patients, addressing any questions or concerns that may arise.
In conclusion, understanding the observations expected during vagus nerve stimulation is crucial for nurses involved in the care of patients undergoing this therapy. By comprehending the anatomy and function of the vagus nerve, as well as the science behind vagus nerve stimulation, nurses can provide better support and care to their patients. Being aware of the physical, emotional, and psychological responses expected during therapy allows nurses to monitor and address any potential risks or complications adequately. Ultimately, the nurse’s role in preparing the patient and diligently monitoring their responses plays a vital role in the success of vagus nerve stimulation as a therapeutic intervention.
Ready to deepen your understanding of the vagus nerve and harness its power for your health and well-being? Discover the secrets of this remarkable system in the “My Vagus Nerve & Me Book.” Learn about its intricate functions, from regulating your heart rate and digestion to its role in mental health and immune response. Find out how to stimulate your vagus nerve both naturally and artificially, and explore its impact on liver detoxification, blood sugar levels, and more. Embark on a journey to better health by getting your copy of the My Vagus Nerve & Me eBook today!