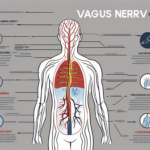
The vagus nerve is a vital component of the autonomic nervous system, responsible for regulating numerous bodily functions. Among its many roles, the vagus nerve plays a crucial part in transmitting impulses to the heart, influencing heart rate and overall cardiovascular health. Understanding the intricacies of this connection can shed light on various physiological processes and potential treatment options for heart-related disorders. In this comprehensive overview, we will delve into the anatomy and function of the vagus nerve, explore its influence on heart rate, discuss neurotransmitter involvement, and examine disorders and future research directions in the field.
Understanding the Vagus Nerve
Anatomy and Function of the Vagus Nerve
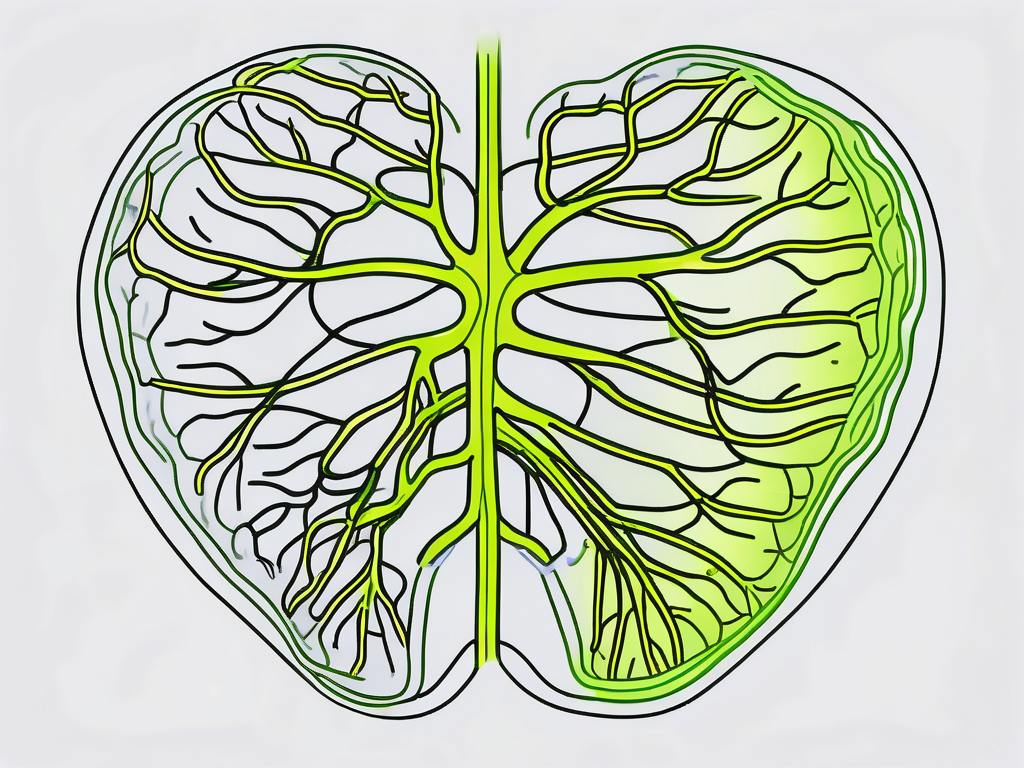
The vagus nerve, also known as the tenth cranial nerve, is the longest and most complex of the cranial nerves. It originates in the brainstem and consists of approximately 80% afferent fibers, which transmit sensory information from the body to the brain, and 20% efferent fibers, which carry motor commands from the brain to various organs, including the heart.
Functionally, the vagus nerve is divided into two main branches: the sensory and motor fibers. The sensory fibers receive information from the organs, such as the heart, lungs, and digestive system, and relay it to the brain. This intricate network of sensory fibers allows the brain to continuously monitor and regulate the body’s internal environment, ensuring optimal functioning and homeostasis.
Conversely, the motor fibers carry commands from the brain to regulate organ function, including heart rate, digestion, and respiratory rate. The vagus nerve plays a crucial role in maintaining the delicate balance between the sympathetic and parasympathetic nervous systems, allowing for precise control of bodily functions.
The Vagus Nerve’s Role in the Autonomic Nervous System
To understand the vagus nerve’s influence on the heart, it is essential to grasp its position within the autonomic nervous system (ANS). The ANS is responsible for controlling involuntary bodily functions, such as heart rate, blood pressure, digestion, and breathing.
The ANS is further divided into two branches: the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS). The SNS is responsible for the “fight-or-flight” response, which prepares the body for action in times of stress or danger. When faced with a perceived threat, the SNS activates, increasing heart rate, dilating blood vessels, and redirecting blood flow to the muscles, enabling a rapid response.
On the other hand, the PNS, regulated by the vagus nerve, oversees the body’s “rest-and-digest” response, promoting relaxation and restoration. When the body is in a state of calm, the PNS takes over, reducing heart rate, constricting blood vessels, and enhancing digestion and nutrient absorption. This intricate dance between the SNS and PNS, orchestrated by the vagus nerve, ensures that the body can adapt and respond appropriately to various situations.
Moreover, the vagus nerve’s influence extends beyond the heart and digestive system. It also plays a vital role in regulating respiratory function. The motor fibers of the vagus nerve innervate the muscles involved in breathing, allowing for precise control of respiratory rate and depth. This intricate coordination ensures that oxygen is efficiently delivered to the body’s tissues and carbon dioxide is effectively eliminated.
Furthermore, recent research has uncovered the vagus nerve’s involvement in various other bodily functions, such as immune regulation, inflammation control, and even mood regulation. The vagus nerve acts as a communication highway between the brain and the body, transmitting signals that influence overall well-being and health.
In conclusion, the vagus nerve, with its intricate network of sensory and motor fibers, plays a crucial role in maintaining homeostasis and regulating vital bodily functions. From its influence on heart rate and digestion to its involvement in the autonomic nervous system and beyond, the vagus nerve’s significance cannot be overstated. Understanding the complexities of this remarkable nerve opens up new avenues for research and potential therapeutic interventions to enhance human health and well-being.
The Vagus Nerve and Heart Connection
How the Vagus Nerve Influences Heart Rate
One of the primary roles of the vagus nerve in the cardiovascular system is its modulation of heart rate. When the body is at rest, the parasympathetic nervous system (PNS), via the vagus nerve, lowers heart rate to maintain a steady and efficient rhythm.
Through the release of the neurotransmitter acetylcholine, the vagus nerve stimulates muscarinic receptors in the heart, which inhibits the firing rate of the sinoatrial (SA) node – the heart’s natural pacemaker. This inhibition slows down the electrical impulses that initiate each heartbeat, resulting in a decrease in heart rate. By regulating heart rate in this way, the vagus nerve helps ensure that the heart functions optimally even during periods of rest and relaxation.
Furthermore, the vagus nerve contributes to the dynamic control of heart rate during physical exertion or emotional stress. In such situations, the sympathetic nervous system (SNS) takes center stage, increasing heart rate to meet the body’s increased demand for oxygen and nutrients. The SNS releases norepinephrine, a neurotransmitter that binds to beta-adrenergic receptors in the heart, leading to an increase in heart rate and cardiac output.
The Impact of Vagus Nerve Stimulation on the Heart
Vagus nerve stimulation (VNS) is a therapeutic technique that involves the use of electrical impulses to stimulate the vagus nerve. It has shown promising results in various cardiovascular conditions, such as heart failure and arrhythmias.
Through targeted electrical stimulation, VNS can enhance the vagus nerve’s activity and subsequently affect heart rate variability, blood pressure, and cardiac contractility. By increasing vagal tone, VNS promotes a more balanced autonomic nervous system response, which can be beneficial for individuals with certain heart conditions.
Research has demonstrated that VNS can improve heart rate variability, which is an important marker of cardiovascular health. Heart rate variability refers to the variation in the time interval between consecutive heartbeats, and higher variability is associated with better cardiovascular fitness and resilience. VNS achieves this by modulating the activity of the vagus nerve, which plays a crucial role in maintaining heart rate variability.
In addition to heart rate variability, VNS has also been shown to have positive effects on blood pressure regulation. By stimulating the vagus nerve, VNS can help lower blood pressure in individuals with hypertension. This effect is achieved through the vagus nerve’s influence on the relaxation of blood vessels and the reduction of sympathetic activity.
Furthermore, VNS can impact cardiac contractility, which refers to the strength and efficiency with which the heart pumps blood. By enhancing vagal tone, VNS can improve the coordination and strength of the heart’s contractions, leading to better overall cardiac function.
However, it is crucial to note that VNS should only be administered under the guidance of a medical professional and after assessing potential risks and benefits specific to each individual’s condition. While VNS holds promise as a therapeutic intervention for certain cardiovascular conditions, its use should be carefully considered and tailored to the needs of each patient.
Neurotransmitters and the Vagus Nerve
The vagus nerve plays a crucial role in the regulation of various bodily functions, including heart rate and digestion. One of the primary neurotransmitters involved in transmitting signals along the vagus nerve is acetylcholine (ACh).
Role of Acetylcholine in Vagus Nerve Function
Acetylcholine is responsible for transmitting signals along the vagus nerve, exerting its effects on various organs, including the heart and gastrointestinal tract.
When acetylcholine is released from the vagal efferent fibers, it has a significant impact on cardiac function. It helps regulate heart rate, ensuring that it remains within a normal range. This neurotransmitter acts as an inhibitory signal, slowing down the heart rate when necessary.
Beyond its role in heart rate regulation, acetylcholine released by the vagus nerve also affects the gastrointestinal tract. It plays a crucial role in promoting digestion by influencing smooth muscle contractions and the secretion of digestive enzymes and fluids. This ensures that food is properly broken down and absorbed by the body.
Impact of Neurotransmitter Imbalance on Heart Function
An imbalance in neurotransmitter levels, including acetylcholine, can have adverse effects on heart function. When there is a dysregulation of the vagus nerve’s inhibitory influence on the heart, it can lead to various cardiac conditions.
Tachycardia, which is characterized by an abnormally fast heart rate, can occur when there is an excess of acetylcholine or when the vagus nerve is overactive. On the other hand, bradycardia, which is characterized by an abnormally slow heart rate, can occur when there is a deficiency of acetylcholine or when the vagus nerve is underactive.
In addition to abnormal heart rates, an imbalance in acetylcholine levels can also contribute to arrhythmias, which are irregular heart rhythms. These conditions can have significant implications for overall cardiovascular health and should not be ignored.
If you experience any irregularities in heart rate or suspect vagus nerve-related issues, it is crucial to consult with a healthcare professional. They will be able to provide you with a proper evaluation and guidance on appropriate diagnostic measures and potential treatment options. Early detection and intervention can help manage these conditions effectively and prevent further complications.
Disorders Related to the Vagus Nerve and Heart
Vagus Nerve Dysfunction and Heart Disease
Vagus nerve dysfunction can manifest in various ways, potentially impacting heart health and function. Disorders such as autonomic neuropathy and vagal neuropathy can disrupt the vagus nerve’s regulation of heart rate, potentially leading to cardiovascular complications.
The vagus nerve, also known as the tenth cranial nerve, plays a crucial role in regulating the body’s involuntary functions, including heart rate, digestion, and breathing. When the vagus nerve malfunctions, it can result in an imbalance in the autonomic nervous system, which controls these essential bodily processes.
Autonomic neuropathy refers to damage or dysfunction of the autonomic nerves, including the vagus nerve. This condition can be caused by various factors, such as diabetes, autoimmune diseases, or certain medications. When the vagus nerve is affected by autonomic neuropathy, it may fail to transmit signals properly, leading to irregular heart rate or other cardiovascular issues.
Similarly, vagal neuropathy specifically refers to damage or dysfunction of the vagus nerve. This condition can occur due to trauma, infections, or underlying medical conditions. When the vagus nerve is impaired, it may result in an inability to regulate heart rate effectively, potentially contributing to the development of heart disease.
Individuals with cardiovascular issues, such as heart disease or arrhythmias, should consult with their healthcare provider to assess the possible involvement of the vagus nerve and explore appropriate treatment options. Understanding the role of the vagus nerve in heart health can help healthcare professionals develop targeted treatment plans to address the underlying causes of these disorders.
Treatment Options for Vagus Nerve-Related Disorders
The treatment of vagus nerve-related disorders varies depending on the underlying cause and severity of symptoms. Approaches may include medication to regulate heart rate or manage associated conditions, lifestyle modifications, and, in some cases, surgical interventions.
Medications such as beta-blockers or anti-arrhythmic drugs may be prescribed to regulate heart rate and minimize the impact of vagus nerve dysfunction on cardiovascular health. These medications work by blocking the effects of certain neurotransmitters or by stabilizing the electrical signals in the heart.
Lifestyle modifications can also play a significant role in managing vagus nerve-related disorders. Engaging in regular exercise, maintaining a healthy diet, managing stress levels, and avoiding triggers that may exacerbate symptoms can help improve heart health and overall well-being.
In some cases, surgical interventions may be necessary to address severe vagus nerve dysfunction. Procedures such as vagus nerve stimulation or surgical repair of damaged nerve fibers can be considered to restore proper functioning of the vagus nerve and alleviate associated symptoms.
It is important to note that treatment decisions should be made in consultation with healthcare professionals who can provide personalized recommendations based on an individual’s unique medical history, symptoms, and diagnostic findings. Each case of vagus nerve-related disorders is unique, and a comprehensive approach is necessary to ensure the most effective and appropriate treatment plan.
Future Research Directions
Potential Therapeutic Applications of Vagus Nerve Stimulation
The field of vagus nerve research continues to evolve, and ongoing studies explore the potential therapeutic applications of vagus nerve stimulation beyond heart-related conditions. Researchers are investigating its potential role in the management of chronic inflammatory diseases, mental health disorders, and even possible implications in neurodegenerative diseases.
One area of interest is the potential use of vagus nerve stimulation in the treatment of chronic inflammatory diseases such as rheumatoid arthritis and Crohn’s disease. Inflammation plays a crucial role in the pathogenesis of these conditions, and researchers believe that by modulating the activity of the vagus nerve, it may be possible to reduce inflammation and alleviate symptoms.
Furthermore, there is growing evidence suggesting that vagus nerve stimulation may have a positive impact on mental health disorders. Studies have shown promising results in the treatment of depression, anxiety, and post-traumatic stress disorder (PTSD) through the use of vagus nerve stimulation. By targeting specific areas of the brain involved in mood regulation, this therapy has the potential to revolutionize the field of mental health treatment.
In addition to its potential therapeutic applications in chronic inflammatory diseases and mental health disorders, vagus nerve stimulation is also being explored for its possible implications in neurodegenerative diseases such as Alzheimer’s and Parkinson’s disease. These conditions are characterized by the progressive loss of neuronal function, and researchers believe that by stimulating the vagus nerve, it may be possible to slow down or even halt the neurodegenerative process.
Unanswered Questions in Vagus Nerve and Heart Research
While significant progress has been made in understanding the vagus nerve’s role in heart function, many questions remain unanswered. Researchers continue to explore the precise mechanisms underlying the complex interplay between the vagus nerve and the cardiovascular system, opening avenues for further exploration and potential breakthroughs in the future.
One area of ongoing research is the identification of specific neurotransmitters involved in the vagus nerve’s regulation of heart rate. While it is known that acetylcholine plays a key role in slowing down heart rate, there may be other neurotransmitters involved in this process that have yet to be discovered. Understanding the full range of neurotransmitters involved could lead to the development of more targeted therapies for heart conditions.
Another unanswered question is the potential role of the vagus nerve in the development of cardiac arrhythmias. While it is known that vagus nerve stimulation can cause bradycardia (slow heart rate), its involvement in the development of arrhythmias such as atrial fibrillation is still not fully understood. Further research is needed to elucidate the mechanisms by which the vagus nerve influences cardiac rhythm and to explore potential therapeutic interventions.
In conclusion, the vagus nerve’s impact on the heart is a complex and multi-faceted relationship. Its role in regulating heart rate, neurotransmitter involvement, and potential disorders highlights the significance of comprehensive understanding and ongoing research. As our knowledge of the vagus nerve continues to expand, so too will our ability to develop innovative therapies for a wide range of conditions. If you have any concerns regarding heart health or vagus nerve-related issues, it is vital to consult with healthcare professionals who can guide you through appropriate diagnostics, treatments, and management strategies tailored to your specific needs.
If you’re fascinated by the critical role the vagus nerve plays in heart health and overall well-being, as detailed in this comprehensive overview, you’ll find the “My Vagus Nerve & Me Book” an invaluable resource. Dive deeper into the world of this remarkable nerve system that orchestrates functions from heart rate regulation to immune response. Discover the secrets of stimulating your vagus nerve to enhance your health naturally. Embrace the opportunity to learn more about this vital aspect of your physiology. Get My Vagus Nerve & Me eBook today and embark on a journey to better health and understanding.