The vagus nerve is an important component of the human body’s nervous system, playing a crucial role in the regulation of various bodily functions. When this nerve is damaged, it can have a significant impact on a person’s overall health and well-being. In this comprehensive guide, we will explore the various aspects of testing for vagus nerve damage, including understanding the role of the vagus nerve, common symptoms of damage, medical tests used for diagnosis, interpreting test results, treatment options, and living with vagus nerve damage.
Understanding the Vagus Nerve
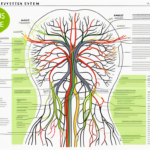
The vagus nerve, also known as the tenth cranial nerve, is the longest and most complex cranial nerve in the body. It originates in the brainstem and extends down into the abdomen, innervating various organs along its pathway. The vagus nerve is responsible for regulating a wide range of bodily functions, including heart rate, digestion, respiratory rate, and even emotional responses.
Damage to the vagus nerve can disrupt the normal functioning of these bodily processes, leading to a variety of symptoms and health complications. Identifying and assessing vagus nerve damage requires a thorough understanding of the nerve’s role in the body and the associated symptoms that may arise.
The Role of the Vagus Nerve in the Body
The vagus nerve carries information between the brain and several key organs, including the heart, lungs, stomach, and intestines. It helps regulate heart rate, controlling the balance between the sympathetic and parasympathetic nervous systems. The parasympathetic division of the vagus nerve promotes rest and relaxation, slowing down heart rate and reducing blood pressure. This intricate regulation ensures that the body maintains a steady state, allowing for optimal functioning.
Additionally, the vagus nerve plays a vital role in digestion, stimulating the release of enzymes and promoting peristalsis, the rhythmic contractions that move food through the intestines. It also helps regulate the function of the liver, pancreas, and gallbladder. Without the vagus nerve, the digestive system would struggle to break down food and absorb nutrients efficiently.
Furthermore, the vagus nerve is involved in vocalization and facial expressions, contributing to social interactions and emotional well-being. It allows us to communicate our thoughts and feelings through speech and express our emotions through facial expressions. This connection between the vagus nerve and our ability to communicate and connect with others highlights its importance in our daily lives.
Given its involvement in these critical bodily functions, damage to the vagus nerve can give rise to a variety of symptoms depending on the specific area affected. Understanding these symptoms is crucial in diagnosing and treating vagus nerve damage effectively.
Common Symptoms of Vagus Nerve Damage
Vagus nerve damage can manifest in a wide range of symptoms due to its extensive innervation throughout the body. Some common symptoms may include:
- Heart palpitations or irregular heartbeat: The vagus nerve helps regulate heart rate, so damage to the nerve can cause disruptions in the heart’s rhythm.
- Dizziness or lightheadedness: The vagus nerve plays a role in maintaining blood pressure, so damage to the nerve can lead to changes in blood flow and feelings of dizziness.
- Difficulty swallowing or a sensation of choking: The vagus nerve controls the muscles involved in swallowing, so damage to the nerve can affect this process.
- Nausea or vomiting: The vagus nerve is involved in the regulation of the digestive system, so damage to the nerve can lead to disruptions in the normal functioning of the stomach and intestines.
- Changes in bowel movements, such as diarrhea or constipation: The vagus nerve helps regulate the movement of food through the intestines, so damage to the nerve can result in changes in bowel habits.
- Abdominal pain or bloating: The vagus nerve innervates the abdominal organs, so damage to the nerve can cause discomfort and pain in the abdomen.
- Hoarse voice or voice changes: The vagus nerve controls the muscles involved in vocalization, so damage to the nerve can affect the voice.
- Difficulty in regulating body temperature: The vagus nerve plays a role in the regulation of body temperature, so damage to the nerve can disrupt this process.
- Anxiety or depression: The vagus nerve is connected to the emotional centers in the brain, so damage to the nerve can impact emotional well-being.
If you experience any of these symptoms, it is important to consult with a medical professional to determine the underlying cause and appropriate course of action. While these symptoms can be indicative of vagus nerve damage, they may also be associated with other conditions, so a thorough evaluation is necessary for an accurate diagnosis.
Medical Tests for Vagus Nerve Damage
In order to diagnose vagus nerve damage, healthcare providers may utilize a combination of physical examinations, neurological tests, and imaging studies. These various tests aim to assess the function and integrity of the vagus nerve and identify any abnormalities or injuries.
Physical Examination
During a physical examination, a healthcare provider may evaluate specific symptoms associated with vagus nerve damage. They may check for abnormal heart rhythms, assess reflexes, and examine the throat, neck, and abdominal areas for any signs of muscle weakness or abnormalities. Additionally, they may perform tests to evaluate the function of other organs that the vagus nerve innervates, such as the lungs and digestive system.
For example, the healthcare provider may listen to the patient’s heart using a stethoscope to detect any irregularities in heart rate or rhythm. They may also use a reflex hammer to test the patient’s reflexes, tapping on specific areas of the body to observe the response. Furthermore, they may gently palpate the neck and throat to feel for any lumps, swelling, or tenderness that could indicate vagus nerve damage.
In addition to these examinations, the healthcare provider may ask the patient about their symptoms and medical history. This comprehensive approach helps gather important information that can aid in the diagnosis of vagus nerve damage.
Neurological Tests
Neurological tests are designed to assess the function of the nervous system, including the vagus nerve. These tests may include assessing sensation, muscle strength, and reflexes. For example, a healthcare provider may use electrodiagnostic tests, such as electromyography (EMG) or nerve conduction studies, to measure electrical activity in the muscles and nerves.
During an EMG, small electrodes are inserted into the muscles to record their electrical activity. This test can help determine if there is any damage or dysfunction in the muscles controlled by the vagus nerve. Nerve conduction studies involve the placement of electrodes on the skin to measure the speed and strength of electrical signals traveling along the nerves. These tests can provide valuable information about the health and function of the vagus nerve.
Another commonly used test is the autonomic reflex screen, which evaluates the autonomic nervous system’s response to various stimuli. This test can provide valuable information about the functioning of the vagus nerve and its impact on heart rate, blood pressure, sweating, and other autonomic functions.
Imaging Tests
Imaging tests, such as magnetic resonance imaging (MRI) or computed tomography (CT) scans, may be utilized to visualize the structures surrounding the vagus nerve. These imaging studies can help identify any structural abnormalities, such as tumors, lesions, or compressions, which may be causing vagus nerve damage.
During an MRI, a powerful magnetic field and radio waves are used to create detailed images of the body’s internal structures. This can help healthcare providers identify any anatomical changes or abnormalities in the vicinity of the vagus nerve. CT scans, on the other hand, use a series of X-ray images taken from different angles to produce cross-sectional images of the body. These scans can provide valuable information about the structures surrounding the vagus nerve and help pinpoint the cause of nerve damage.
Additionally, ultrasound may be used to assess blood flow and measure the diameter of the vagus nerve. This non-invasive imaging technique uses high-frequency sound waves to create real-time images of the body’s internal structures. By visualizing the vagus nerve and assessing its blood flow, healthcare providers can gain further insights into the extent of nerve damage and potential underlying causes.
Interpreting Test Results
After undergoing the necessary tests, a medical professional will evaluate the results to determine the presence and extent of vagus nerve damage. Interpreting these test results requires expertise and a comprehensive understanding of the underlying pathology. To ensure an accurate diagnosis, it is essential to consult with a knowledgeable healthcare provider who can explain the findings and their implications.
The evaluation of test results for vagus nerve damage involves a thorough analysis of various factors. The medical professional will carefully examine the test data, including nerve conduction studies, electromyography, and imaging scans. They will assess the amplitude, latency, and conduction velocity of nerve signals, looking for any abnormalities or disruptions in the vagus nerve pathway.
Furthermore, the medical professional will consider the patient’s medical history, symptoms, and any other relevant information. This comprehensive approach helps in understanding the context of the test results and provides a more accurate interpretation.
Understanding Medical Reports
Medical reports can be complex and filled with technical jargon. It is important to consult with a medical professional who can explain the findings and their significance in simple terms. They can clarify any uncertainties and address any questions or concerns you may have. Remember that self-diagnosis and self-interpretation of medical reports can lead to incorrect conclusions and unnecessary stress.
When reviewing a medical report related to vagus nerve damage, it is crucial to have a clear understanding of the terminology used. The report may include terms such as “nerve conduction velocity,” “amplitude,” “latency,” and “electromyography.” A healthcare provider can explain these terms and their relevance to your specific case, ensuring that you have a comprehensive understanding of the report.
Additionally, the medical professional can provide insights into the potential causes of vagus nerve damage, such as trauma, inflammation, or underlying medical conditions. Understanding the underlying factors can help you make informed decisions about your treatment options and lifestyle modifications.
When to Seek a Second Opinion
If you have received a diagnosis of vagus nerve damage or are unsure about the interpretation of your test results, it is always advisable to seek a second opinion. Consulting with another healthcare professional can provide you with a fresh perspective and ensure that you are receiving the most accurate and appropriate care. They may suggest additional tests or diagnostic procedures to further investigate your condition and confirm the initial diagnosis.
Seeking a second opinion is particularly important when the test results are inconclusive or when the proposed treatment plan raises concerns. Another healthcare provider can review your medical history, test results, and symptoms to offer a different viewpoint. This process can help you gain confidence in your diagnosis and treatment plan, providing peace of mind and ensuring that you are on the right path to recovery.
Remember, seeking a second opinion is not a sign of mistrust but rather a proactive approach to your healthcare. It allows you to explore different perspectives and make well-informed decisions about your treatment and overall well-being.
Treatment Options for Vagus Nerve Damage
Treatment options for vagus nerve damage depend on the underlying cause and the severity of the damage. It is important to note that there is no specific medication or surgical intervention targeted solely at repairing the vagus nerve itself. However, managing the symptoms and addressing the underlying cause can help alleviate the impact of vagus nerve damage on overall health.
Medication and Drug Therapy
In some cases, medications may be prescribed to manage specific symptoms associated with vagus nerve damage. For example, anti-arrhythmic medications may be used to regulate heart rhythms, while medications for acid reflux or gastroparesis can help alleviate stomach-related symptoms. It is important to carefully follow the prescribed medication regimen and consult with a healthcare professional regarding any potential side effects or interactions.
When it comes to vagus nerve damage, medication can be a valuable tool in symptom management. By targeting specific symptoms, such as irregular heart rhythms or digestive issues, medications can help individuals lead a more comfortable and functional life. It is crucial to work closely with a healthcare professional to find the right medication and dosage for each individual’s unique needs.
While medications can provide relief, it is important to remember that they do not directly repair the vagus nerve itself. Instead, they aim to alleviate symptoms and improve overall well-being. It is essential to have realistic expectations and understand that medication is just one component of a comprehensive treatment plan for vagus nerve damage.
Physical Therapy and Rehabilitation
Physical therapy and rehabilitation programs can play a crucial role in optimizing the recovery and function of individuals with vagus nerve damage. These programs may focus on strengthening muscles, improving coordination, and addressing any difficulties with swallowing or speech. Additionally, certain relaxation techniques, such as deep breathing exercises, can stimulate the vagus nerve and promote overall well-being.
Physical therapy is a non-invasive and effective approach to managing vagus nerve damage. Through targeted exercises and techniques, physical therapists can help individuals regain strength, improve mobility, and enhance overall quality of life. These programs are tailored to each individual’s specific needs and can be adjusted as progress is made.
In addition to physical therapy, rehabilitation programs may also include occupational therapy and speech therapy. Occupational therapists can assist individuals in adapting to daily activities and regaining independence, while speech therapists can help with any difficulties related to speech and swallowing. These multidisciplinary approaches ensure a comprehensive and holistic approach to vagus nerve damage treatment.
Surgical Interventions
In severe cases of vagus nerve damage, surgical interventions may be considered. However, these procedures are typically targeted at treating the underlying cause rather than directly repairing the vagus nerve itself. Potential surgical options may include repairing or removing tumors, relieving nerve compressions, or reconstructing damaged structures.
Surgery is generally reserved for cases where conservative treatments have not provided sufficient relief or when there is a clear structural issue that needs to be addressed. It is important to note that surgical interventions for vagus nerve damage are highly specialized and should only be performed by experienced surgeons with expertise in this area.
Before considering surgery, individuals will undergo a thorough evaluation to determine the most appropriate course of action. This evaluation may include imaging tests, such as MRI or CT scans, to assess the extent of the damage and identify any potential surgical targets. The decision to undergo surgery should be made in close consultation with a healthcare professional, taking into account the potential risks and benefits.
While surgical interventions can be effective in certain cases, it is important to remember that they do not directly repair the vagus nerve itself. Instead, they aim to address the underlying cause of the damage and alleviate symptoms. Rehabilitation and ongoing management may still be necessary after surgery to optimize recovery and long-term outcomes.
Living with Vagus Nerve Damage
Vagus nerve damage can have a significant impact on a person’s daily life. The vagus nerve, also known as the “wandering nerve,” is a crucial part of the autonomic nervous system that regulates various bodily functions, including heart rate, digestion, and breathing. When this nerve is damaged, it can lead to a wide range of symptoms and challenges.
However, there are various strategies and resources available to help individuals manage their condition and improve their overall well-being. It’s important to note that every person’s experience with vagus nerve damage is unique, and what works for one individual may not work for another. It is essential to consult with healthcare professionals to develop a personalized treatment plan.
Lifestyle Changes and Home Remedies
Making certain lifestyle changes and adopting specific home remedies can provide relief for individuals with vagus nerve damage. One of the key aspects is adopting a healthy diet. Including foods rich in omega-3 fatty acids, such as salmon and walnuts, can help reduce inflammation and support nerve health. Additionally, incorporating stress-reducing activities into daily routines, such as engaging in regular physical activity, practicing deep breathing exercises, and ensuring adequate sleep, can have a positive impact on overall well-being.
Alternative therapies have also shown promise in managing vagus nerve damage. Acupuncture, for example, involves the insertion of thin needles into specific points on the body to stimulate the nervous system and promote healing. Yoga and meditation, on the other hand, focus on relaxation techniques and mindfulness, helping individuals manage stress and improve their mental well-being. It is important to consult with a healthcare professional before implementing any home remedies or alternative therapies to ensure they are safe and suitable for individual needs.
Psychological Impact and Coping Strategies
Living with vagus nerve damage can be challenging both physically and emotionally. It is not uncommon for individuals to experience anxiety, depression, or other psychological symptoms as a result of their condition. The constant battle with pain, discomfort, and uncertainty can take a toll on mental health.
Seeking support from mental health professionals can be invaluable in managing the psychological impact of vagus nerve damage. Therapies such as cognitive-behavioral therapy (CBT) can help individuals develop coping strategies and address negative thought patterns. Relaxation techniques, such as progressive muscle relaxation or guided imagery, can also provide relief and promote a sense of calmness.
Support Groups and Resources
Connecting with others who are experiencing similar challenges can provide a sense of understanding, support, and empowerment. Support groups, both in-person and online, offer opportunities to share experiences, exchange information, and learn from others. Hearing stories of resilience and finding a community that understands the daily struggles can be incredibly comforting.
Additionally, there are numerous online resources, educational websites, and reputable organizations dedicated to providing information and support for individuals with vagus nerve damage and their caregivers. These resources offer a wealth of knowledge about the condition, treatment options, and self-care strategies. They can also provide updates on the latest research and advancements in the field, empowering individuals to stay informed and take an active role in their healthcare journey.
In conclusion, living with vagus nerve damage requires a multifaceted approach to manage symptoms and improve overall well-being. Lifestyle changes, home remedies, psychological support, and connecting with support groups and resources can all play a significant role in helping individuals navigate the challenges they face. It is important to remember that each person’s journey is unique, and consulting with healthcare professionals is essential for personalized diagnosis, treatment, and support.
If you’re fascinated by the remarkable capabilities of the vagus nerve and its profound impact on your health, “My Vagus Nerve & Me Book” is the perfect resource to deepen your understanding. Discover the intricacies of this complex system, from regulating your heart rate to supporting liver detoxification. Learn practical ways to stimulate your vagus nerve, both naturally and artificially, to enhance your well-being. Take the first step towards harnessing the power of your body’s most astonishing nerve. Get My Vagus Nerve & Me eBook today and embark on a journey to optimal health.