The vagus nerve is a complex and vital part of our nervous system. It plays a significant role in various bodily functions, including pain perception. In this comprehensive guide, we will explore the anatomy and function of the vagus nerve, understand the causes and symptoms of vagus nerve pain, delve into the diagnosis and treatment options available, discuss preventive measures, and provide insights for living with vagus nerve pain. Remember, while this guide aims to inform and educate, it is crucial to consult with a healthcare professional for personalized advice and treatment.
Understanding the Vagus Nerve
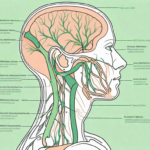
The vagus nerve, also known as the tenth cranial nerve, is the longest and most complex nerve in our bodies. It originates in the brainstem and meanders down through the neck, chest, and abdomen. This vital nerve branches out to various organs, including the heart, lungs, and digestive system, playing a crucial role in regulating their functions.
The vagus nerve is a fascinating part of our anatomy, with a rich history of scientific discovery. It was first described by the ancient Roman physician Galen, who named it “vagus,” meaning “wandering” in Latin, due to its extensive and meandering course throughout the body. Since then, researchers have been captivated by the intricate connections and functions of this remarkable nerve.
Anatomy and Function of the Vagus Nerve
Comprising both sensory and motor fibers, the vagus nerve is responsible for transmitting information between the brain and various organs. It controls processes such as heart rate, digestion, inflammation response, and vocalization. The vagus nerve also enables the parasympathetic nervous system, which promotes a state of rest and digest.
One of the most intriguing aspects of the vagus nerve is its extensive network of connections. As it travels through the body, it sends out branches that innervate not only the major organs but also smaller structures, such as the larynx, pharynx, and esophagus. These connections allow for the coordination of complex functions, such as swallowing, speaking, and even influencing our emotional state.
The Role of the Vagus Nerve in Pain Perception
The vagus nerve carries sensory information from organs to the brain, including pain signals. When there is dysfunction or irritation of the vagus nerve, it can lead to vagus nerve pain, also known as vagus neuralgia. Conditions such as inflammation, trauma, infection, or compression can contribute to the onset of vagus nerve pain.
Understanding the role of the vagus nerve in pain perception is an area of active research. Scientists are investigating how the nerve communicates pain signals and how it interacts with other pain pathways in the body. By unraveling these mechanisms, researchers hope to develop new treatments for chronic pain conditions that involve the vagus nerve.
Furthermore, recent studies have suggested that stimulating the vagus nerve can have therapeutic effects. Vagus nerve stimulation (VNS) has been used to treat various conditions, including epilepsy and depression. By delivering electrical impulses to the nerve, VNS can modulate its activity and potentially alleviate symptoms.
As our understanding of the vagus nerve continues to expand, so does our appreciation for its intricate role in our overall well-being. From regulating our heart rate to influencing our emotional state, this wandering nerve holds the key to numerous physiological processes. Exploring its complexities not only deepens our knowledge of human anatomy but also opens up new avenues for medical advancements.
Causes of Vagus Nerve Pain
Vagus nerve pain, also known as vagal neuralgia, can be a debilitating condition that affects many individuals. It is important to understand the various causes of this pain in order to effectively prevent and manage it.
The vagus nerve, also called the tenth cranial nerve, is a vital component of the autonomic nervous system. It plays a crucial role in regulating many bodily functions, including heart rate, digestion, and breathing. When the vagus nerve becomes irritated or inflamed, it can lead to discomfort and pain.
Medical Conditions Associated with Vagus Nerve Pain
There are several medical conditions that have been linked to vagus nerve pain. One such condition is migraine headaches. Migraines are intense, throbbing headaches that can be accompanied by nausea, vomiting, and sensitivity to light and sound. The exact mechanism by which migraines cause vagus nerve pain is not fully understood, but it is believed that the inflammation and vascular changes associated with migraines can irritate the vagus nerve.
Gastroesophageal reflux disease (GERD) is another medical condition that can contribute to vagus nerve pain. GERD occurs when stomach acid flows back into the esophagus, causing a burning sensation in the chest, known as heartburn. The acid reflux can irritate the vagus nerve, leading to pain and discomfort.
Irritable bowel syndrome (IBS) is a common gastrointestinal disorder that can also be associated with vagus nerve pain. Individuals with IBS often experience abdominal pain, bloating, and changes in bowel habits. The exact relationship between IBS and vagus nerve pain is not fully understood, but it is believed that the abnormal contractions of the intestines in IBS can irritate the vagus nerve.
Fibromyalgia, a chronic pain condition characterized by widespread musculoskeletal pain, fatigue, and sleep disturbances, has also been linked to vagus nerve pain. The exact cause of fibromyalgia is unknown, but it is believed that abnormalities in the central nervous system, including the vagus nerve, play a role in the development of this condition.
Lifestyle Factors Contributing to Vagus Nerve Pain
Aside from medical conditions, lifestyle factors can also contribute to vagus nerve dysfunction and pain. Chronic stress, for example, can have a profound impact on the functioning of the vagus nerve. When we experience stress, the body’s fight-or-flight response is activated, leading to increased heart rate, elevated blood pressure, and decreased digestive function. This response is regulated by the vagus nerve. Prolonged stress can cause the vagus nerve to become overstimulated, leading to pain and discomfort.
Poor sleep quality and duration can also affect the vagus nerve. During sleep, the body undergoes important restorative processes, including the regulation of the autonomic nervous system. When sleep is disrupted or inadequate, the vagus nerve may not function optimally, leading to pain and discomfort.
Sedentary behavior, such as sitting for long periods of time, can negatively impact the vagus nerve. Physical activity helps stimulate the vagus nerve and promotes its proper functioning. Engaging in regular exercise, such as walking, swimming, or yoga, can help support vagus nerve health and reduce the risk of pain.
Lastly, an unhealthy diet can contribute to vagus nerve dysfunction. Consuming foods that are high in sugar, unhealthy fats, and processed ingredients can lead to inflammation in the body, including the vagus nerve. On the other hand, a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can help reduce inflammation and support overall nerve health.
In conclusion, vagus nerve pain can arise from various medical conditions and lifestyle factors. Understanding these causes is crucial in order to effectively prevent and manage this debilitating condition. By addressing medical conditions, adopting a healthy lifestyle, and seeking appropriate medical care, individuals can support vagus nerve health and reduce the risk of pain and discomfort.
Symptoms of Vagus Nerve Pain
Vagus nerve pain can manifest in various ways, affecting both physical and emotional well-being. Understanding the symptoms associated with vagus nerve dysfunction can help individuals seek appropriate medical attention and support.
Physical Symptoms of Vagus Nerve Dysfunction
Physical symptoms of vagus nerve dysfunction can be diverse and may vary in severity. One common physical symptom is chest pain, which can range from mild discomfort to intense pressure or tightness in the chest. This sensation can be alarming and may lead individuals to seek immediate medical attention.
Heart palpitations are another physical symptom that individuals with vagus nerve dysfunction may experience. These palpitations can feel like a racing or irregular heartbeat, causing individuals to feel their heart pounding in their chest. It is important to note that heart palpitations can also be a symptom of other medical conditions, so a thorough evaluation is necessary to determine the underlying cause.
Difficulty swallowing, also known as dysphagia, is another physical symptom associated with vagus nerve dysfunction. This can manifest as a feeling of food getting stuck in the throat or a sensation of choking while eating or drinking. It is essential to address this symptom promptly, as it can lead to malnutrition and dehydration if left untreated.
Gastrointestinal issues are also common physical symptoms of vagus nerve dysfunction. These issues can include nausea, vomiting, bloating, and abdominal pain. Individuals may experience changes in bowel movements, such as constipation or diarrhea, which can significantly impact their quality of life.
Lightheadedness is another physical symptom that individuals with vagus nerve dysfunction may encounter. This can manifest as a feeling of dizziness, unsteadiness, or faintness. It is crucial to take precautions to prevent falls and injuries, especially when lightheadedness occurs unexpectedly.
While these physical symptoms can be distressing, it is important to remember that they are indicative of an underlying issue that can be addressed with appropriate medical care and treatment.
Emotional and Psychological Effects of Vagus Nerve Pain
Vagus nerve pain can have a significant impact on emotional and psychological well-being. The vagus nerve plays a crucial role in regulating the body’s stress response and emotional state, so dysfunction in this nerve can lead to various emotional and psychological challenges.
Anxiety is a common emotional symptom experienced by individuals with vagus nerve pain. It can manifest as excessive worry, restlessness, irritability, and a sense of impending doom. These symptoms can significantly interfere with daily functioning and quality of life.
Depression is another emotional symptom that individuals with vagus nerve dysfunction may experience. It can manifest as persistent feelings of sadness, hopelessness, and a loss of interest in activities once enjoyed. Depression can be debilitating and may require a combination of therapy and medication to manage effectively.
Mood swings are also common in individuals with vagus nerve dysfunction. These swings can range from feeling elated and energetic to feeling irritable and low. Understanding and managing these mood fluctuations can be challenging, but with appropriate support, individuals can find strategies to cope.
Difficulties with concentration and memory are also associated with vagus nerve pain. Individuals may find it challenging to focus on tasks, retain information, or recall memories. This can impact work, relationships, and overall cognitive functioning.
Seeking support from mental health professionals can be beneficial in managing the emotional and psychological effects of vagus nerve pain. Therapies such as cognitive-behavioral therapy (CBT) and mindfulness techniques can help individuals develop coping strategies and improve their overall well-being.
In conclusion, vagus nerve pain can manifest in various physical and emotional symptoms. It is essential to seek medical evaluation and support to address these symptoms effectively and improve overall quality of life.
Diagnosis of Vagus Nerve Pain
Accurate diagnosis is crucial for effective management of vagus nerve pain. Healthcare professionals employ various methods to evaluate and identify the underlying causes.
Medical History and Physical Examination
When it comes to diagnosing vagus nerve pain, medical professionals take a comprehensive approach. They will begin by reviewing your medical history and performing a thorough physical examination. This allows them to assess your symptoms, identify potential triggers, and rule out other conditions with similar manifestations.
During the medical history review, it is essential to provide detailed information about your symptoms, medical history, and any relevant lifestyle factors. This information helps the healthcare professional gain a better understanding of your overall health and any potential factors that may be contributing to your vagus nerve pain.
Following the medical history review, a physical examination will be conducted. This examination may involve assessing your vital signs, such as heart rate and blood pressure, as well as examining specific areas of your body that may be affected by vagus nerve pain. The healthcare professional will carefully evaluate your physical condition, looking for any signs or symptoms that may indicate vagus nerve dysfunction.
Diagnostic Tests for Vagus Nerve Dysfunction
In some cases, healthcare professionals may order diagnostic tests to further study the vagus nerve’s function and determine the root cause of vagus nerve pain.
One common diagnostic test is an electrocardiogram (ECG). This test measures the electrical activity of your heart and can help identify any irregularities or abnormalities that may be affecting the vagus nerve. By analyzing the ECG results, healthcare professionals can gain valuable insights into the functioning of the vagus nerve and its potential role in your pain.
In addition to an ECG, imaging scans may also be ordered to provide a more detailed view of the vagus nerve and surrounding structures. Magnetic resonance imaging (MRI) or computed tomography (CT) scans can help identify any structural abnormalities or nerve compression that may be contributing to your symptoms.
Nerve conduction studies are another diagnostic tool that can be used to assess the function of the vagus nerve. During this test, small electrodes are placed on your skin, and a mild electrical current is applied to stimulate the nerve. The healthcare professional can then measure the speed and strength of the electrical signals transmitted by the vagus nerve, providing valuable information about its functioning.
By combining the information gathered from the medical history review, physical examination, and diagnostic tests, healthcare professionals can make a more accurate diagnosis of vagus nerve pain. This diagnosis is crucial for developing an effective management plan tailored to your specific needs.
Treatment Options for Vagus Nerve Pain
Multiple treatment options are available for managing vagus nerve pain. It is important to consult with a healthcare professional to find the most appropriate treatment plan for your individual circumstances.
When it comes to vagus nerve pain relief, there are various approaches that can be taken. These approaches can be broadly categorized into two main categories: medications and non-pharmacological therapies. Each of these categories offers different benefits and can be tailored to suit the specific needs of the individual.
Medications for Vagus Nerve Pain Relief
Medications such as anti-inflammatory drugs, analgesics, and anticonvulsants may be prescribed to alleviate pain and reduce inflammation. These medications work by targeting the underlying causes of vagus nerve pain, providing relief and improving overall quality of life.
Anti-inflammatory drugs, such as nonsteroidal anti-inflammatory drugs (NSAIDs), can help reduce inflammation and relieve pain associated with vagus nerve pain. These medications work by inhibiting the production of certain chemicals in the body that cause inflammation. By reducing inflammation, these drugs can help alleviate pain and discomfort.
Analgesics, commonly known as painkillers, can also be used to manage vagus nerve pain. These medications work by blocking the transmission of pain signals to the brain, providing temporary relief from pain. They can be effective in managing mild to moderate pain associated with vagus nerve pain.
Anticonvulsants, which are primarily used to treat seizures, can also be prescribed to manage vagus nerve pain. These medications work by stabilizing the electrical activity in the brain, reducing the occurrence of abnormal nerve impulses that can cause pain. By regulating the nerve activity, anticonvulsants can help alleviate pain and improve overall nerve function.
Your healthcare provider will assess your symptoms and medical profile to determine the most effective medication for your condition. They will take into account factors such as the severity of your pain, the underlying cause of the vagus nerve pain, and any other medical conditions you may have. It is important to follow your healthcare provider’s instructions and take the prescribed medication as directed.
Non-Pharmacological Therapies for Vagus Nerve Pain
Non-pharmacological therapies can complement medical treatments for vagus nerve pain relief. These therapies focus on alternative approaches to managing pain and promoting overall well-being. They can be used in conjunction with medications or as standalone treatments, depending on the individual’s needs and preferences.
Physical therapy is a commonly recommended non-pharmacological therapy for vagus nerve pain. It involves exercises and techniques that aim to improve strength, flexibility, and mobility. Physical therapists can design personalized exercise programs to target specific areas affected by vagus nerve pain, helping to reduce pain and improve overall function.
Acupuncture is another non-pharmacological therapy that has been used for centuries to manage pain. This ancient Chinese practice involves the insertion of thin needles into specific points on the body to stimulate the flow of energy and promote healing. Acupuncture has been found to be effective in reducing pain and improving overall well-being in individuals with vagus nerve pain.
Relaxation techniques, such as deep breathing exercises, meditation, and yoga, can also be beneficial for managing vagus nerve pain. These techniques help promote relaxation, reduce stress, and improve overall mental and physical well-being. By reducing stress and promoting relaxation, these techniques can help alleviate pain and improve overall quality of life.
Cognitive-behavioral therapy (CBT) is a type of therapy that focuses on changing negative thought patterns and behaviors. It can be helpful for individuals with vagus nerve pain who may be experiencing anxiety or depression as a result of their condition. CBT can help individuals develop coping strategies, manage pain-related stress, and improve overall psychological well-being.
Additionally, adopting a healthy lifestyle and stress reduction techniques can provide significant benefits for vagus nerve health. This may include regular exercise, a balanced diet, adequate sleep, and stress management techniques such as mindfulness and relaxation exercises.
It is important to note that the effectiveness of non-pharmacological therapies may vary from person to person. It is recommended to consult with a healthcare professional to determine the most appropriate non-pharmacological therapy for your specific needs and to ensure proper guidance and supervision throughout the treatment process.
Preventing Vagus Nerve Pain
Prevention plays a crucial role in maintaining vagus nerve health.
Lifestyle Modifications for Vagus Nerve Health
Adopting healthy habits such as regular exercise, proper nutrition, stress reduction techniques, and adequate sleep can support overall nerve health, including the vagus nerve. These lifestyle modifications can reduce the risk and severity of vagus nerve pain.
Regular Check-ups and Early Detection
Regular check-ups with your healthcare provider can help monitor your overall health and identify any potential issues with the vagus nerve. Early detection of problems can lead to timely intervention and improved outcomes.
Living with Vagus Nerve Pain
Chronic pain can significantly impact an individual’s quality of life. Adopting coping strategies and seeking support can help individuals manage the challenges associated with vagus nerve pain.
Coping Strategies for Chronic Pain
Managing chronic pain involves finding coping strategies that work for you. These may include relaxation techniques, mindfulness, engaging in hobbies, and seeking support from friends, family, or support groups. It is essential to develop a personalized plan and explore what works best for your specific needs.
Support and Resources for Individuals with Vagus Nerve Pain
Seeking support from others who share similar experiences can provide comfort and valuable insights. Online communities, support groups, and counseling services can connect individuals with vagus nerve pain to helpful resources and emotional support.
In conclusion, understanding the anatomy, function, causes, symptoms, diagnosis, and treatment options of vagus nerve pain can empower individuals to take proactive steps in managing their health. By adopting healthy lifestyle habits, seeking medical advice, and exploring appropriate treatment options, individuals can effectively navigate their vagus nerve pain journey and improve their overall well-being.
If you’re inspired to take your understanding of the vagus nerve to the next level, “My Vagus Nerve & Me Book” is the perfect companion on your journey to better health. Dive deep into the complexities of this remarkable nerve and discover practical ways to stimulate it for improved well-being. From immune system support to heart rate regulation and mental health, this book covers it all. Embrace the power of knowledge and Get My Vagus Nerve & Me eBook today to unlock the secrets of one of the most fascinating systems in your body.