The vagus nerve is an essential component of our nervous system, playing a crucial role in regulating many bodily functions. But what happens when this important nerve becomes damaged? Can a vagus nerve be repaired? In this article, we will delve into the world of the vagus nerve, exploring its function, causes of damage, symptoms, diagnosing methods, treatment options, and the possibility of repairing this vital nerve.
Understanding the Vagus Nerve
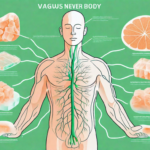
Just what is the vagus nerve and why is it so important? The vagus nerve, also known as the tenth cranial nerve, is the longest cranial nerve in the body. It originates in the brainstem and extends all the way down to the abdomen, innervating various organs along the way. The vagus nerve is responsible for regulating numerous bodily functions, including heart rate, digestion, breathing, and even certain aspects of cognition and mood.
The vagus nerve is a complex and fascinating part of the human body. It plays a crucial role in maintaining the delicate balance of our physiological processes. Let’s delve deeper into the intricate workings of this remarkable nerve.
The Role and Function of the Vagus Nerve
The vagus nerve acts as a communication highway between the brain and the rest of the body. It carries vital information back and forth, ensuring smooth coordination and functioning of various bodily systems. One of its key functions is to help maintain the body’s homeostasis, or the optimal balance of physiological processes. It achieves this through its parasympathetic branch, which promotes relaxation, restoration, and digestion.
When we experience stress or danger, the sympathetic nervous system kicks into gear, preparing our body for fight or flight. However, once the threat has passed, the vagus nerve takes over, activating the parasympathetic branch to calm us down and restore equilibrium. This branch of the vagus nerve slows down our heart rate, stimulates digestion, and promotes a sense of relaxation.
Furthermore, the vagus nerve plays a significant role in our emotional well-being. It is involved in regulating mood and emotions, with studies suggesting that stimulating the vagus nerve can help alleviate symptoms of depression and anxiety. This connection between the vagus nerve and mental health highlights its importance beyond its physical functions.
The Anatomy of the Vagus Nerve
The vagus nerve consists of both motor and sensory fibers. The motor fibers control the muscles that allow for swallowing and speech, while the sensory fibers relay information from the organs back to the brain. This intricate network of communication enables seamless coordination of bodily functions.
As the vagus nerve travels down from the brainstem, it branches out to innervate various organs, including the heart, lungs, liver, stomach, and intestines. This extensive reach allows the vagus nerve to exert its influence over a wide range of bodily processes.
Interestingly, recent research has also uncovered the role of the vagus nerve in the gut-brain connection. The gut is often referred to as the “second brain” due to its extensive network of neurons. The vagus nerve acts as a vital link between the gut and the brain, facilitating bidirectional communication. This connection has implications for our overall health, as disruptions in the gut-brain axis have been linked to various conditions, including irritable bowel syndrome and mood disorders.
In conclusion, the vagus nerve is a remarkable and multifaceted component of our nervous system. Its role in regulating physiological processes, maintaining homeostasis, and influencing our emotional well-being cannot be overstated. Understanding the intricacies of the vagus nerve opens up new avenues for research and potential therapeutic interventions.
Causes of Vagus Nerve Damage
While the vagus nerve is resilient, there are several factors that can lead to its damage. These causes can be broadly categorized into physical trauma and diseases/conditions affecting the nerve.
Physical Trauma and the Vagus Nerve
Physical trauma, such as a severe blow to the head or neck, can result in acute damage to the vagus nerve. The vagus nerve, being one of the longest and most complex nerves in the body, extends from the brainstem down to the abdomen, innervating various organs along the way. Therefore, any trauma to the head or neck region can potentially affect the vagus nerve’s function.
In some cases, injury to nearby structures, such as the spine or blood vessels, can also affect the nerve’s function. For example, a fracture or dislocation of the cervical spine can put pressure on the vagus nerve, leading to dysfunction. Similarly, damage to the blood vessels that supply the nerve can compromise its blood flow and cause damage.
It’s important to seek immediate medical attention if you experience any trauma to the head or neck to assess the extent of the damage to the vagus nerve. Prompt diagnosis and treatment can help prevent further complications and promote recovery.
Diseases and Conditions Affecting the Vagus Nerve
Several diseases and conditions can impact the vagus nerve, leading to dysfunction or damage. Chronic conditions such as diabetes or autoimmune disorders may gradually affect the nerve’s function over time. In the case of diabetes, high blood sugar levels can cause damage to the nerves, including the vagus nerve, leading to a condition called diabetic neuropathy.
Infections, tumors, or inflammation in the vicinity of the nerve can also cause compression or damage. For instance, a viral infection like shingles can affect the nerves, including the vagus nerve, causing pain and dysfunction. Similarly, tumors growing near the nerve can put pressure on it, leading to symptoms such as difficulty swallowing or hoarseness of voice.
Furthermore, autoimmune disorders, where the immune system mistakenly attacks the body’s own tissues, can also affect the vagus nerve. Conditions like Guillain-Barré syndrome, in which the immune system attacks the peripheral nerves, including the vagus nerve, can result in weakness, numbness, and other neurological symptoms.
It is important for individuals with known risk factors or symptoms suggestive of vagus nerve damage to consult with a healthcare professional for proper evaluation and management. Treatment options may include medications, physical therapy, or in some cases, surgical intervention.
Symptoms of Vagus Nerve Damage
Vagus nerve damage can manifest in various ways, depending on the extent of the injury and the specific functions impaired. The symptoms can be divided into physical and psychological symptoms.
Physical Symptoms of Vagus Nerve Damage
Physical symptoms may include difficulty swallowing or speaking, a weak voice, hoarseness, changes in heart rate or blood pressure, problems with digestion such as reflux or gastroparesis, and issues with bowel movements.
Difficulty swallowing or dysphagia is a common physical symptom of vagus nerve damage. This can make it challenging to eat or drink, leading to weight loss or malnutrition if not properly managed. Additionally, individuals may experience discomfort or pain while swallowing, which can be distressing and impact their overall quality of life.
Another physical symptom is a weak voice or hoarseness. The vagus nerve plays a crucial role in controlling the muscles responsible for vocalization. When damaged, these muscles may not function properly, resulting in a weakened voice or hoarseness. This can make communication difficult and affect social interactions.
Changes in heart rate or blood pressure are also common physical symptoms of vagus nerve damage. The vagus nerve helps regulate heart rate and blood pressure, so any disruption in its function can lead to irregularities in these vital signs. Individuals may experience rapid heart rate, low blood pressure, or fluctuations in both, which can cause dizziness, lightheadedness, or fainting spells.
Problems with digestion, such as reflux or gastroparesis, can occur when the vagus nerve is damaged. Reflux, also known as gastroesophageal reflux disease (GERD), is characterized by the backward flow of stomach acid into the esophagus. This can cause heartburn, chest pain, and difficulty swallowing. Gastroparesis, on the other hand, is a condition where the stomach takes longer than usual to empty its contents into the small intestine. This can lead to bloating, nausea, vomiting, and a feeling of fullness even after eating small amounts of food.
Issues with bowel movements can also arise from vagus nerve damage. The vagus nerve helps regulate the movement of food through the digestive tract. When damaged, it can result in constipation, diarrhea, or a combination of both. These bowel irregularities can cause discomfort, abdominal pain, and impact overall bowel function.
Psychological Symptoms of Vagus Nerve Damage
Psychological symptoms can vary widely, but may include changes in mood or cognition, anxiety, depression, or problems with memory and concentration. It’s important to note that psychological symptoms alone may not be indicative of vagus nerve damage and should be assessed by a healthcare professional.
Changes in mood or affect can occur when the vagus nerve is damaged. Individuals may experience heightened irritability, mood swings, or emotional instability. These changes in mood can impact relationships and overall well-being.
Cognitive difficulties, such as problems with memory and concentration, can also be observed in individuals with vagus nerve damage. The vagus nerve plays a role in cognitive function, and when impaired, individuals may struggle with memory recall, attention span, and processing information. This can affect daily activities, work performance, and academic achievements.
Anxiety and depression are common psychological symptoms associated with vagus nerve damage. The vagus nerve is involved in regulating the body’s stress response and mood. When damaged, individuals may experience heightened anxiety, excessive worry, or feelings of sadness and hopelessness. These psychological symptoms can significantly impact an individual’s mental health and overall quality of life.
It’s important to recognize that psychological symptoms alone may not be solely attributed to vagus nerve damage. Other factors, such as underlying mental health conditions or external stressors, can contribute to these symptoms. Therefore, a comprehensive evaluation by a healthcare professional is essential to determine the underlying cause and appropriate treatment plan.
Diagnosing Vagus Nerve Damage
Diagnosing vagus nerve damage can be a complex process, as symptoms can be non-specific and overlap with other conditions. Healthcare professionals typically start by taking a comprehensive medical history and conducting a thorough physical examination.
Medical History and Physical Examination
A detailed medical history helps to identify potential causes of vagus nerve damage, such as past injuries, medical conditions, or lifestyle factors. For example, a history of trauma to the neck or chest area, such as a car accident or a sports injury, may increase the likelihood of vagus nerve damage. Additionally, certain medical conditions like diabetes, autoimmune disorders, or previous surgeries in the neck or chest region can also contribute to nerve damage.
During the physical examination, the healthcare professional may assess various functions controlled by the vagus nerve, such as heart rate, blood pressure, and swallowing ability. They may use specialized tools, such as a stethoscope to listen to the heart and lungs, or a blood pressure cuff to measure blood pressure. By evaluating these functions, the healthcare professional can gather important clues about the health of the vagus nerve.
Diagnostic Tests for Vagus Nerve Damage
In some cases, additional diagnostic tests may be required to evaluate the extent of the nerve damage. These tests may include imaging studies, such as magnetic resonance imaging (MRI) or computed tomography (CT) scans, to visualize the nerve and surrounding structures. These imaging techniques can provide detailed images of the neck and chest area, allowing healthcare professionals to identify any abnormalities or damage to the vagus nerve.
Electrophysiological tests, such as electromyography (EMG) or nerve conduction studies, can provide valuable information about the nerve’s function. During an EMG, small electrodes are placed on the skin to measure the electrical activity of the muscles controlled by the vagus nerve. This test can help determine if the nerve is sending appropriate signals to the muscles. Nerve conduction studies involve the placement of electrodes on the skin to measure the speed and strength of electrical signals as they travel along the vagus nerve. These tests can help pinpoint the location and severity of the nerve damage.
In addition to these tests, healthcare professionals may also perform specialized tests to evaluate specific functions of the vagus nerve. For example, a swallowing study may be conducted to assess the nerve’s role in swallowing and identify any difficulties or abnormalities. This study typically involves swallowing various substances, such as liquid or solid materials, while the healthcare professional monitors the movement of the substances through the esophagus.
Overall, diagnosing vagus nerve damage requires a comprehensive approach that combines medical history, physical examination, and various diagnostic tests. By gathering as much information as possible, healthcare professionals can accurately assess the extent of the nerve damage and develop an appropriate treatment plan.
Treatment Options for Vagus Nerve Damage
Treatment for vagus nerve damage depends on the underlying cause, severity of symptoms, and individual patient factors. It’s essential to consult with a healthcare professional to determine the most suitable treatment plan.
The vagus nerve, also known as the cranial nerve X, is a crucial component of the autonomic nervous system. It plays a vital role in regulating various bodily functions, including digestion, heart rate, and breathing. When the vagus nerve is damaged, it can lead to a range of symptoms, such as difficulty swallowing, voice hoarseness, heart rhythm abnormalities, and gastrointestinal issues.
In cases of mild vagus nerve damage, non-surgical treatments may be recommended. These can include dietary modifications, medications to manage specific symptoms such as acid reflux or gastroparesis, physical therapy to improve swallowing and voice function, and lifestyle changes to reduce stress levels.
Dietary modifications can involve avoiding certain foods that may trigger symptoms, such as spicy or fatty foods. Instead, a healthcare professional may recommend a diet rich in fiber, fruits, and vegetables to promote healthy digestion. Additionally, they may suggest eating smaller, more frequent meals to alleviate symptoms of gastroparesis, a condition characterized by delayed stomach emptying.
Medications can be prescribed to manage specific symptoms associated with vagus nerve damage. For example, proton pump inhibitors or H2 blockers may be used to reduce acid reflux, while prokinetic agents can help improve gastrointestinal motility in cases of gastroparesis.
Physical therapy can play a crucial role in rehabilitating the vagus nerve and improving swallowing and voice function. Therapists can employ various techniques, such as exercises to strengthen the muscles involved in swallowing or vocal cord exercises to enhance voice quality.
Lifestyle changes, such as stress reduction techniques and relaxation exercises, can also be beneficial in managing vagus nerve damage. Stress can exacerbate symptoms and hinder the healing process, so finding healthy coping mechanisms and incorporating relaxation techniques into daily routines can be helpful.
In more severe cases, surgical interventions may be necessary to repair or bypass the damaged portion of the vagus nerve. However, the feasibility and success of surgical treatments for vagus nerve damage depend on various factors, including the extent and location of the injury, overall health of the patient, and individual response to surgical interventions.
Surgical options for vagus nerve damage can include nerve grafting, where a healthy nerve is taken from another part of the body and used to repair the damaged section of the vagus nerve. Another surgical approach is nerve stimulation, where an electrical device is implanted to stimulate the vagus nerve and restore its function.
It’s important to note that surgical treatments for vagus nerve damage are typically reserved for severe cases that do not respond to non-surgical interventions. The decision to undergo surgery should be made in close consultation with a healthcare professional, weighing the potential risks and benefits.
In conclusion, treatment options for vagus nerve damage range from non-surgical approaches, such as dietary modifications, medications, physical therapy, and lifestyle changes, to surgical interventions like nerve grafting and nerve stimulation. The choice of treatment depends on the severity of symptoms, underlying cause, and individual patient factors. Consulting with a healthcare professional is crucial in determining the most appropriate treatment plan for vagus nerve damage.
The Possibility of Vagus Nerve Repair
Repairing the vagus nerve is a complex challenge, mainly due to its delicate nature and the elaborate network of connections it forms throughout the body. While nerve repair and regeneration are areas of active research, the current understanding and capabilities in vagus nerve repair are still limited.
The vagus nerve, also known as the “wandering nerve,” is the longest cranial nerve in the body. It extends from the brainstem to various organs, including the heart, lungs, stomach, and intestines. This extensive distribution allows the vagus nerve to play a crucial role in regulating a wide range of bodily functions, such as heart rate, digestion, and even mood.
When the vagus nerve is damaged, whether due to trauma, surgery, or disease, it can lead to significant disruptions in these vital functions. Restoring the function of the vagus nerve is therefore of great importance in improving the quality of life for individuals affected by such damage.
The Science Behind Nerve Repair
Nerve repair involves reconnecting damaged nerve fibers to restore their function. Regeneration of nerve fibers can occur naturally to some extent, but it is often incomplete, leading to functional deficits. Researchers are exploring various strategies to enhance nerve repair, including the use of scaffolds, growth factors, and innovative surgical techniques.
Scaffolds are biocompatible materials that provide a framework for nerve regeneration. They can be designed to mimic the natural extracellular matrix, providing structural support and promoting the growth of new nerve fibers. Growth factors, on the other hand, are substances that stimulate the growth and differentiation of nerve cells. By delivering these factors directly to the damaged area, researchers hope to enhance the regeneration process.
Innovative surgical techniques, such as nerve grafting and nerve transfer, are also being investigated. Nerve grafting involves taking a segment of a healthy nerve from another part of the body and using it to bridge the gap in the damaged nerve. Nerve transfer, on the other hand, involves rerouting a healthy nerve to the damaged area, allowing it to take over the function of the damaged nerve.
Challenges in Vagus Nerve Repair
Repairing the vagus nerve presents unique challenges due to its extensive distribution and complex connections. The intricate anatomy and function of the nerve make it difficult to achieve complete regeneration and restoration of normal function. However, advancements in technology and understanding hold promise for future breakthroughs.
One of the challenges in vagus nerve repair is the potential for the formation of scar tissue. Scar tissue can impede the regeneration process and hinder the reestablishment of proper nerve function. Researchers are investigating ways to minimize scar formation and promote a favorable environment for nerve regeneration.
Another challenge lies in the precise reconnection of the numerous branches and fibers of the vagus nerve. Each branch of the nerve may have different functions and connections, making it crucial to accurately restore the intricate network. Researchers are exploring advanced imaging techniques and surgical approaches to improve the precision of nerve repair.
Furthermore, the vagus nerve interacts with various other systems in the body, including the immune system and the gut microbiota. These interactions can influence the regenerative process and the overall success of vagus nerve repair. Understanding these complex interactions is essential for developing effective strategies for nerve repair.
In conclusion, while the repair of the vagus nerve poses significant challenges, ongoing research and advancements in technology offer hope for future breakthroughs. By unraveling the complexities of nerve regeneration and developing innovative approaches, scientists aim to restore the function of the vagus nerve and improve the lives of individuals affected by its damage.
The Future of Vagus Nerve Repair
While repairing the vagus nerve remains a complex and ongoing challenge, significant advancements in medical technology offer hope for the future.
Advances in Medical Technology
Emerging technologies, such as nerve tissue engineering and neurostimulation, are opening new avenues for nerve repair and regeneration. Researchers are exploring the use of stem cells, artificial constructs, and electrical stimulation to enhance nerve healing and functional recovery.
Potential Breakthroughs in Vagus Nerve Repair
Ongoing research into neuroregeneration and neuroplasticity holds potential for future breakthroughs in vagus nerve repair. By further understanding the mechanisms involved in nerve repair and exploring innovative treatment approaches, the medical community aims to improve outcomes for individuals with vagus nerve damage.
Conclusion
In conclusion, repairing the vagus nerve remains a complex and challenging task. The vagus nerve plays a vital role in regulating various bodily functions, and its damage can have significant consequences. While current treatment options focus on managing symptoms, researchers continue to explore ways to repair and regenerate the damaged vagus nerve. If you experience any symptoms or suspect vagus nerve damage, it is crucial to consult with a healthcare professional who can provide an accurate diagnosis and guide you towards the most appropriate treatment options.
If you’re fascinated by the incredible capabilities of the vagus nerve and its impact on your health, “My Vagus Nerve & Me Book” offers a wealth of knowledge to deepen your understanding. Discover the secrets of one of the most sophisticated systems within your body, and learn practical ways to stimulate your vagus nerve for improved well-being. Whether you’re seeking to enhance your immune system, optimize digestion, or maintain a healthy heart rate and mental health, this book is an invaluable resource. Don’t miss out on the opportunity to unlock the full potential of your vagus nerve. Get My Vagus Nerve & Me eBook today and take the first step towards harnessing the power of your body’s natural processes.